What is Hypermobility and Ehlers-Danlos Syndrome
Hypermobility is a condition where joints have a larger range of motion than normal, and is sometimes referred to as being ‘double-jointed’. It can result in joint pain, fatigue, stiffness, and instability, especially when it’s a part of Ehlers-Danlos Syndrome (EDS).
Ehlers-Danlos Syndrome is a group of inherited connective tissue disorders that are characterised by stretchy skin, joint hypermobility, and tissue fragility.
Why the Upper Neck and Jaw Matter More Than You Think
When people talk about hypermobility or Ehlers-Danlos Syndrome (EDS), the focus is often on bendy joints, stretchy skin, and widespread pain. However, two areas that are frequently overlooked, yet profoundly important, are the upper neck (upper cervical spine) and the jaw (temporomandibular joint, or TMJ).
These regions play a major role in stability, nervous system function, and everyday comfort. For many people with hypermobility or EDS, dysfunction here can cause symptoms far beyond simple neck stiffness or jaw clicking. Common complaints include dizziness, headaches, visual changes, tinnitus (ringing in the ears), nausea, brain fog, and even digestive symptoms.
Understanding Hypermobility and EDS
Joint hypermobility means that joints move beyond the typical range of motion. For some people, this flexibility is harmless.
For others, particularly those with Ehlers-Danlos Syndrome (EDS) or Hypermobility Spectrum Disorder (HSD), this flexibility comes with consequences. These may include joint instability, fragile connective tissue, chronic pain, fatigue, and widespread systemic symptoms.
EDS is a group of genetic conditions affecting collagen, the body’s main structural protein. Because collagen is present throughout the body in ligaments, fascia, blood vessels, skin, and organs, symptoms can affect many systems at once.
The Upper Neck’s Role in EDS: Restriction and Dysfunction
The upper cervical spine, made up of C0 (base of the skull), C1 (atlas), and C2 (axis), is one of the most neurologically sensitive areas in the body. These small but critical joints:
- Protect the brainstem
- Influence balance and eye movement
- Help regulate blood pressure and pain processing
- Provide a large portion of the neck’s total movement
For healthy function, this area requires precise mobility and stability.
Surrounding these joints are the suboccipital muscles, which contain the highest concentration of muscle spindles in the body. These muscles act as fast-responding sensors, helping the nervous system understand head position and maintain stability.
Hypermobility Does Not Always Mean “Too Loose”
A common and often surprising pattern in EDS is that, despite being globally hypermobile, the upper neck often becomes restricted and guarded.

Why does this happen?
- Deep stabilising muscles fatigue easily
- The body compensates with muscle tension
- Suboccipital muscles develop chronic spasm
- Joint alignment becomes altered
Over time, this protective tension can lead to persistent restriction, altered nerve signalling, and central sensitisation. This may contribute to symptoms such as chronic headaches, migraines, dizziness, nausea, brain fog, and heightened pain sensitivity.
The Watson Headache Approach (Cervicogenic Headache) — A Key Concept in EDS
The Watson Headache model describes headaches that originate in the upper neck, particularly the C1–C3 segments. These headaches are especially common in people with EDS and hypermobility because:
- Upper cervical joints are often unstable
- Deep stabilisers fatigue quickly
- The suboccipital region becomes overloaded and stiff
Many people with EDS experience these symptoms, yet they are frequently misdiagnosed as migraine, anxiety, or unrelated neurological issues.
Signs of Upper Cervical Restriction in EDS
Common indicators include:
- Headaches starting at the base of the skull
- Dizziness, lightheadedness, or a “woozy” feeling
- Neck pain, stiffness, or easy fatigue
- Visual disturbances or eye strain
- A “bobblehead” sensation or needing to support the head
- Nausea or brain fog after turning the head or looking up
The Jaw (TMJ) in Hypermobility and EDS
The temporomandibular joint (TMJ) is small, highly mobile, and heavily dependent on connective tissue — making it particularly vulnerable in hypermobility.
TMJ dysfunction in EDS may include:
- Clicking, popping, or partial dislocation (subluxation)
- Jaw or facial pain
- Ear fullness or tinnitus
- Headaches
- Secondary neck tension
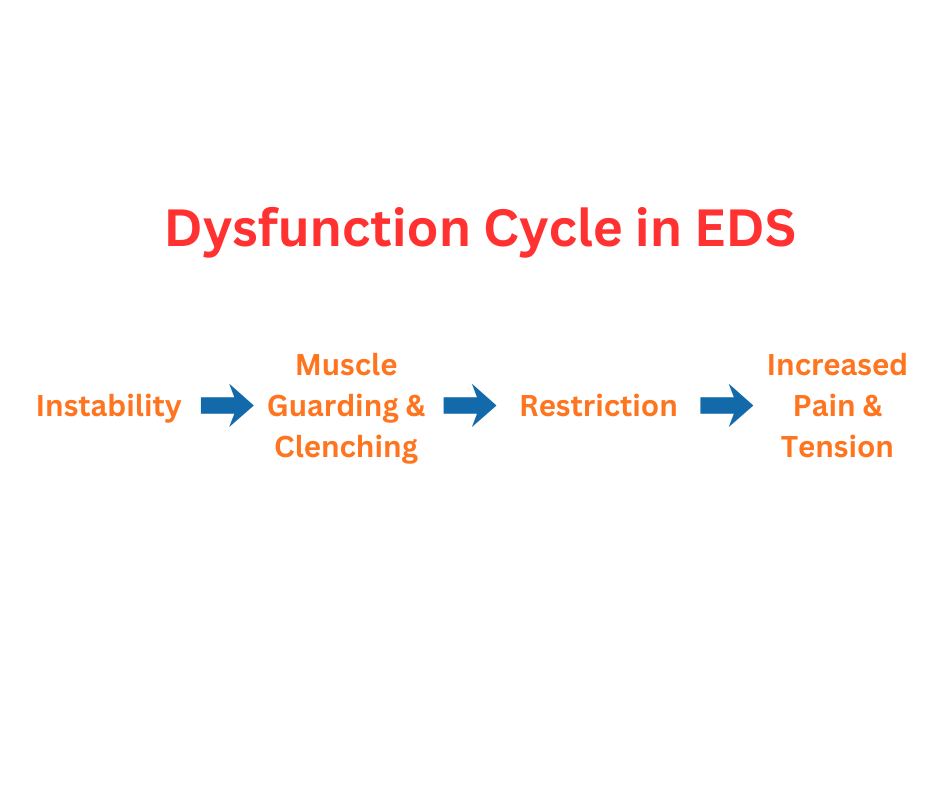
Because the jaw, skull, and upper neck are biomechanically interconnected, dysfunction in one area often aggravates the other. This can create a vicious cycle:
Instability → muscle guarding and clenching → restriction → increased pain and tension
The Neck–Jaw Connection
The upper neck and jaw share muscles, nerves, and fascial connections.
- Tight suboccipital muscles can alter jaw mechanics and overload jaw muscles
- Jaw misalignment can affect head posture and strain the upper neck
- The trigeminocervical complex (where facial and upper neck nerves converge) explains why jaw problems can cause headaches and neck pain — and why upper neck dysfunction can produce facial or jaw pain.
In hypermobility, these interconnected systems tend to fatigue and overload more easily.
Practical Strategies for Managing Neck and Jaw Issues
1. Gentle Stabilisation
- Low-load deep neck flexor exercises
- Controlled jaw stability exercises
- Avoid aggressive stretching of already lax tissues
- Work with a physiotherapist experienced in EDS
2. Posture and Alignment
- Supportive pillows
- Ergonomic work and phone setup
- Avoid prolonged forward-head posture
3. Jaw Care
- Awareness of relaxed jaw and tongue posture
- Avoid hard or chewy foods during symptom flares
- Gentle jaw relaxation techniques
- Abdominal or diaphragmatic breathing
- Consider a TMJ-aware dentist who understands hypermobility
4. Manual Therapy (by EDS-experienced clinicians)

- Gentle myofascial or soft-tissue techniques
- Careful, targeted mobilisation of the upper neck and jaw
- Avoid aggressive mobilisation
In Summary
The upper neck and jaw may be small anatomical regions, but their impact on hypermobility and Ehlers-Danlos Syndrome is enormous.
Recognising upper cervical restriction, cervicogenic headache patterns, and TMJ dysfunction can lead to more accurate diagnosis, better symptom understanding, and more targeted treatment, resulting in an improvement of quality of life.
For targeted physiotherapy treatment to manage jaw and neck issues resulting from hypermobility or EDS, book an appointment with the Headache Neck and Jaw Clinic.

Lisa Eisfeld is a trained physiotherapist from Germany. She has also studied advanced Manual therapy and finished her Osteopathy Diploma in 2018 at the School for Manual Medicine Berlin. Lisa has also attained her Watson Headache Institute Level 1 Foundation and Level 2 Consolidation courses. Read more about Lisa.